For the first time, the tiny fruit fly can be used to study how mutations associated with the development of diabetes affect the production and secretion of the vital hormone insulin.
The advance is due to a new technique devised by researchers at the Stanford University School of Medicine that allows scientists to measure insulin levels in the insects with extremely high sensitivity and reproducibility.
The experimental model is likely to transform the field of diabetes research by bringing the staggering power of fruit fly genetics, honed over 100 years of research, to bear on the devastating condition that affects millions of Americans. Until now, scientists wishing to study the effect of specific mutations on insulin had to rely on the laborious, lengthy and expensive genetic engineering of laboratory mice or other mammals.
In contrast, tiny, short-lived fruit flies can be bred in dizzying combinations by the tens of thousands in just days or weeks in small flasks on a laboratory bench.
"I normally avoid the term, but I think Dr. Park's new technique is a true breakthrough," said Seung Kim, MD, PhD, professor of developmental biology. "Only in selected mammals can researchers measure insulin with this degree of sensitivity."
Kim, who is also a Howard Hughes Medical Institute investigator, is the senior author of the paper describing the research. Research associate Sangbin Park, PhD, is the lead author of the paper, which was published inPLOS Genetics.
The power of a tiny model system
Insulin is an ancient molecule used by nearly all animals to regulate metabolism, growth and development. Diabetes in humans occurs when insulin-making cells in the pancreas fail to produce the hormone or when other cells in the body grow resistant to its effects. In 2002, Kim, his lab team and fellow Stanford researchers discovered that fruit flies develop a diabetes-like condition when their insulin-producing cells are destroyed.
"Studies of diabetes in fruit flies represent a relatively new area of investigation," said Carl Thummel, PhD, professor of human genetics at the University of Utah School of Medicine. Thummel uses the insect to study energy metabolism and metabolic disorders.
"Needless to say, fruit flies are very small, and only tiny amounts of blood can be extracted from their bodies," he said. "Our inability to measure the amounts of circulating insulin has been a major drawback in the field. The technique developed by Dr. Kim's group will allow researchers to rapidly test the effect of diabetes risk factors, and establishes fruit flies as an effective tool for studies of diabetes."
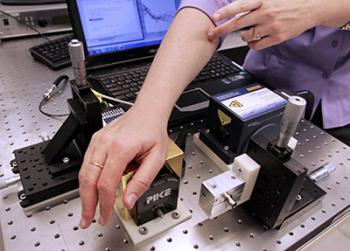
Developed by Park, the new technique uses a chemical tag to label an insulin-like peptide called Ilp2 in fruit flies. The tag allows researchers to use an antibody-based assay to measure insulin concentrations in the insect's blood and cells at the picomolar level - the level at which insulin concentrations are measured in humans.
Using the technique, the researchers were able to quickly identify what a mutation associated with type-2 diabetes in humans actually does: It regulates insulin secretion, but not production.
Understanding the effect of each mutation
Parsing the effect of each mutation on the way the body produces, secretes and responds (or not) to insulin is critical to further understand the disease and to devise new therapeutic approaches. "I was stunned that this technique worked so well to identify the effect of specific mutations," said Park. "Many of the genes we studied seem to have similar functions in governing insulin production or secretion in flies and in humans."
Previous efforts to tag Ilp2 have been hampered by the fact that the protein undergoes a complex series of modifications and folding events on its way to becoming the active form of the molecule. Tags that disrupt this process can cause inappropriate expression of the molecule or render it inactive, interfering with the very metabolic pathway researchers want to study.
Park capitalized on the knowledge that overexpression of the active form of the Ilp2 protein is lethal. He then randomly inserted chemical tags along the length of the molecule to create a panel of molecules tagged in many different places. Testing them individually, he looked for those that were still able to kill the flies - indicating that the molecule's activity had not been compromised. Eventually he found two locations on Ilp2 that were ideal. He could then use antibodies that recognized the tags to quantify levels of Ilp2 with the antibody-based assay.
"Once you know that the modifications, or tags, don't affect the expression or activity of the molecule, you have a lot more power to interpret your experiments," said Kim. "You can begin to track the insulin assembly line, from the transcription of RNA from the gene, to the production of the protein, to the storing and eventual secretion of the protein in response to metabolic signals. You have the opportunity to figure out the mechanisms controlling each of those steps in detail."
In flies, Ilp2 is produced and secreted by specialized neurons in the brain. This makes it relatively easy to compare levels of circulating Ilp2 with the amount of mature but unsecreted Ilp2: simply compare the amount of Ilp2 in the insects' bodies to the amount in their brains.
Park found that the amount of secreted Ilp2 increased from about 0.1 percent to about 0.35 percent of the total available during the first three days of a fruit fly's life. Furthermore, like in humans, circulating Ilp2 concentrations were relatively low in fasting flies, but peaked and then declined after a subsequent meal. Finally he showed that, in flies with only one working copy of the insulin receptor gene (they normally have two, as do humans), insulin secretion was increased in an apparent attempt to compensate for the deficiency - mirroring the development of insulin resistance in humans and mice.
Park and his colleagues then turned their attention to mutations associated with type-2 diabetes in genome-wide studies in humans. These studies don't reveal how a specific mutation might work to affect development of a disease; they show only that people with the condition are more likely than those without it to have certain mutations in their genome. Hundreds of candidate-susceptibility genes have been identified in this way.
Tip of the iceberg
The researchers found that blocking the expression of a fly version of a human protein called GLIS3, known to affect insulin production in mammals, and linked both to type-2 and type-1 diabetes in humans, also affected the production of Ilp2 in flies. A mutation in another protein, BCL11A, was known to be associated with the development of the disease in humans, but its mechanism of action was unclear. Park and his colleagues found that blocking the expression of the fly version of BCL11A did not affect the flies' ability to make Ilp2, but caused it to secrete abnormally high levels of Ilp2 into the bloodstream.
The researchers emphasize that these findings are just the tip of the iceberg. Many more mutations can be studied alone and in combination under a myriad of experimental conditions. A single fruit fly can lay several hundred eggs during its approximately 40-day life span; eggs develop into adults in only 10 days. They plan to continue to use the fruit fly system to complement and inform their ongoing studies in mammals and humans.
"We're really taking advantage of a century of work done by generations of other researchers," said Kim. "Historically the fly has been used to understand developmental biology by looking at its genes and its cells and observing how they change over time. Now we've shown we can accurately and precisely measure levels of a crucial hormone in these insects, and use that to identify new targets for diabetes investigation in mice and humans."
source : http://www.medicalnewstoday.com/releases/280778.php