In the journal Biomedical Optics Express, the team of electrical engineers, from Princeton University, NJ, describes how they used their prototype device to measure blood sugar by directing the laser at a person's palm.
Senior author Claire Gmachl, the Eugene Higgins Professor of Electrical Engineering at Princeton, says:
"With this work we hope to improve the lives of many diabetes sufferers who depend on frequent blood glucose monitoring."
Laser beam penetrates skin and is absorbed by glucose
The device works by sending a laser beam through skin cells - without causing damage - to be absorbed by sugar molecules. The target is not blood sugar as such, but the sugar content of dermal interstitial fluid, which has a strong correlation with blood sugar.
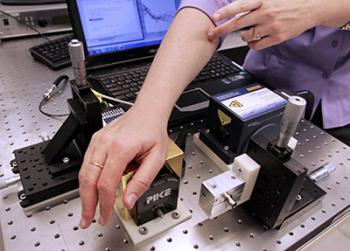
The new monitor uses a laser, instead of blood sample, to read blood sugar levels. The laser is directed at the person's palm, passes through skin cells and is partially absorbed by sugar molecules, allowing researchers to calculate blood sugar levels.
Image credit: Princeton
The amount of absorption of the laser beam is thus an indicator of the amount of glucose in the blood.
The team was surprised at how accurate the readings turned out to be. Current glucose monitors that patients use at home are required to show readings within 20% of the patient's actual blood level.
Lead author Sabbir Liakat, a graduate student in electrical engineering, says even their early version of the laser system met this requirement, and the latest version is 84% accurate.
The challenge now is to improve the technology - and not least to bring down the scale.
When they started working on the idea, the device covered an average lab bench and needed an elaborate system to keep it cool.
Prof. Gmachl says they have solved the cooling problem - the system now works at room temperature - but they still have to work out how to make the technology smaller.
They aim to develop a mobile device they can take to clinics and put through more tests and collect a larger set of data to work with.
The device uses a 'quantum cascade laser' to produce mid-infrared light
The system uses infrared laser light, which is just beyond the spectrum light visible to the human eye. Medical devices currently use near-infrared, a band that has slightly longer wavelengths than the red that the human eye can see. Near-infrared is not blocked by water and can thus be used in the body.
The quantum cascade laser allows the team to select the frequency they need in the mid-infrared region, and also because of recent improvements in the technology, it provides the increased power and stability needed to penetrate the skin.
Image credit: Princeton
But near infrared does not interact with chemicals in the skin - for that you have to move to slightly longer wavelengths in the mid-infrared region. At this wavelength, the laser light is absorbed by blood sugar and is not much affected by other chemicals in the skin.
However, mid-infrared laser light is more difficult to harness with standard lasers, and it also requires higher power and stability in order for the beam to penetrate the skin and scatter off bodily fluid.
But as sometimes happens in projects where people work tirelessly to achieve their goals - there was a breakthrough. This came when they tried a new type of device called a 'quantum cascade laser.'
The quantum cascade laser allows the team to select the frequency they need in the mid-infrared region, and also because of recent improvements in the technology, it provides the increased power and stability needed to penetrate the skin.
Small study shows average readings meet required clinical accuracy
In their study paper they describe how they measured the blood sugar of three healthy volunteers before and after they each ate 20 jellybeans. The researchers also measured the resulting rise in blood sugar with the conventional finger-prick test.
The team repeated the experiment and took measurements several times over several weeks. The results showed that while the laser device's average readings had errors larger than standard blood sugar monitors, they were within the range required for clinical accuracy.
The team is excited by the potential their discovery offers because, as Prof. Gmachl explains, "the quantum cascade laser can be designed to emit light across a very wide wavelength range, its usability is not just for glucose detection, but could conceivably be used for other medical sensing and monitoring applications."
The National Science Foundation, the Wendy and Eric Schmidt Foundation, Daylight Solutions Inc., and Opto-Knowledge Systems helped to fund the study.
Recently, Medical News Today also learned how the discovery of a glucose sensor in the brain may lead to new diabetes treatments.
Non-Invasive Optical Blood Glucose Monitoring System - video
Written by Catharine Paddock PhD
source : http://www.medicalnewstoday.com/articles/281407.php

No comments:
Post a Comment